To yield the three structural proteins capsid, pre-membrane and envelope and the nonstructural proteins, NS1, NS2A, NS2B, NS3, NS4A, 2K, NS4B and NS5. Replication of the DENV genome occurs in intimate association with perinuclear ER membranes which are modified to form characteristic structures during virus infection. High-throughput RNA interference studies have shown that DENV depends heavily on the cellular machinery for replication. However the mechanisms by which DENV interacts with cellular pathways and the viral and cellular proteins involved, largely remain to be determined. Comparative analysis of the gene expression profiles of a range of cell types infected with DENV in vitro and cells isolated from the blood of DENV infected individuals has identified a number of genes and cellular signaling pathways that are specifically dysregulated in DENV infection and may be Sipeimine involved in pathogenesis. In addition, high-throughput interaction studies have identified a number of interactions between DENV and cellular proteins that may play a role in replication or avoiding host defense mechanisms. By contrast to gene expression studies, the analysis of the host response to either DENV or flavivirus infection at the proteomic level is more limited. The standard approach of two-dimensional PAGE combined with the identification of specific proteins by mass spectrometry has been used to  detect proteins that are altered in amount in DENV infected mammalian cells, insect cells and in sera from DENV infected patients and resulted in the identification of a number of cellular proteins potentially relevant to pathogenesis. However this type of analysis is limited by the resolution and sensitivity of 2D-PAGE. In recent years, advances in the sensitivity of MS, coupled with high-throughput protein identification has made it feasible to quantify global Ursolic-acid changes in cellular protein levels in response to viral infection. The use of stable isotope labeling techniques to distinguish proteins derived from different cell populations, either by metabolic labeling of proteins or chemical modification of peptides, in combination with quantitative MS, provides the most sensitive means of accurately analyzing the proteome of a cell currently available. By combining differential labeling techniques with subcellular fractionation and quantitative MS, it is possible not only to measure changes in the amounts of proteins, but also to study changes in the cellular distribution of proteins, even if the total protein levels have not altered significantly. This approach is well suited to the comparative analysis of cell populations such as control and virus infected cells, but surprisingly there are very few reports of the application of these techniques to study viral pathogenesis and none for DENV. In this study we investigated the effects of DENV-2 infection on the host cell proteome of human A549 cells using SILAC in combination with high throughput liquid chromatography MS/MS. The mock and infected A549 cells were fractionated into nuclear and cytoplasmic extracts before analysis to identify proteins that redistribute between cellular compartments during infection and reduce the complexity of the analysis. We identified proteins that both increased and decreased in response to DENV2 infection.
detect proteins that are altered in amount in DENV infected mammalian cells, insect cells and in sera from DENV infected patients and resulted in the identification of a number of cellular proteins potentially relevant to pathogenesis. However this type of analysis is limited by the resolution and sensitivity of 2D-PAGE. In recent years, advances in the sensitivity of MS, coupled with high-throughput protein identification has made it feasible to quantify global Ursolic-acid changes in cellular protein levels in response to viral infection. The use of stable isotope labeling techniques to distinguish proteins derived from different cell populations, either by metabolic labeling of proteins or chemical modification of peptides, in combination with quantitative MS, provides the most sensitive means of accurately analyzing the proteome of a cell currently available. By combining differential labeling techniques with subcellular fractionation and quantitative MS, it is possible not only to measure changes in the amounts of proteins, but also to study changes in the cellular distribution of proteins, even if the total protein levels have not altered significantly. This approach is well suited to the comparative analysis of cell populations such as control and virus infected cells, but surprisingly there are very few reports of the application of these techniques to study viral pathogenesis and none for DENV. In this study we investigated the effects of DENV-2 infection on the host cell proteome of human A549 cells using SILAC in combination with high throughput liquid chromatography MS/MS. The mock and infected A549 cells were fractionated into nuclear and cytoplasmic extracts before analysis to identify proteins that redistribute between cellular compartments during infection and reduce the complexity of the analysis. We identified proteins that both increased and decreased in response to DENV2 infection.
Translation of the genome results in the production of a well established in 4-HNE
Formed by arachidonic acid or other unsaturated fa y acids Tetrahydroberberine following free Benzoylpaeoniflorin radicals a ack, can bind to proteins by Michael addition, with preferential amino acidic binding sites to cysteine, hystidine or lysine residues. Therefore, 4-HNE protein adducts could be considered a reliable OS markers and have a biological impact on protein function. In this regard, the amino acid sequence of the human beta-actin shows several potential 4-HNE binding sites on all the major conformational subdomains of the protein.  A total of 6 C, 8 H and 19 K residues are present in the sequence, and potential 4-HNE binding amino acid residues are present in all the relevant conformational subdomains of the protein, for a total of 2 C, 4 H and 7 K in the subdomain 1, a total of 1 H and 3 K in the subdomain 2, a total of 2 C, 2 H and 5 K in the subdomain 3, and a total of 3 C and 4 K in the subdomain 4. In particular, the subdomain 2 of the molecule is of critical importance for DNAase 1 binding and protein polymerization, while a very crucial C 374 residue and potential binding site for 4-HNE is present in the conformationally critical hydrophobic pocket of the molecule. Our findings indicate that the observed reduction in beta-actin band intensity is independent of the employed monoclonal antibodies and are compatible with a real decrease in the betaactin expression in the R patients erythrocytes membrane. Moreover, the reported evidence exhaustively addresses the question of whether the observed decrease in beta-actin protein expression might be related to oxidative PTMs potentially preventing antibody recognition. Taken together, our data indicate that major alterations exist in the beta-actin of R erythrocytes which results both from changes in expression and as a consequence of oxidative damage. To this regard, beta-actin is a well-known major target for OS processes, while erythrocytes represent ����cellular detectors���� revealing the co-existence of major cytoskeletal changes in this key genetic model for neurodevelopmental disorders. In particular, this work suggests a novel role for MeCP2 as a stabilizing protein in microtubule dynamics. To date, no definitive cure for R exists, although several approaches to a potential therapy have been either a empted or hypothesized, including activation of the silenced Mecp2 gene, gene therapy, modulation of some of the downstream effects from MeCP2-deficiency. Our study indicates that a proteomic approach in R is able to reveal additional downstream effects of the MECP2-deficiency, and therefore could identify potentially novel therapeutical targets for the disease. The four serotypes of dengue virus cause the most important arthropod-borne viral disease of humans. DENV infection results in a range of clinical outcomes ranging from the milder dengue fever to the potentially life threatening dengue haemorrhagic fever/dengue shock syndrome. A recent study estimates that up to 390 million people are infected with DENV annually, making dengue a serious global public-health problem. Despite much effort, there are neither vaccines nor antiviral therapies in clinical use to prevent or treat dengue, and our understanding of dengue pathogenesis is still limited. DENV is a member of the Flavivirus genus of the Flaviviridae family and has a RNA genome of,11 kb in size.
A total of 6 C, 8 H and 19 K residues are present in the sequence, and potential 4-HNE binding amino acid residues are present in all the relevant conformational subdomains of the protein, for a total of 2 C, 4 H and 7 K in the subdomain 1, a total of 1 H and 3 K in the subdomain 2, a total of 2 C, 2 H and 5 K in the subdomain 3, and a total of 3 C and 4 K in the subdomain 4. In particular, the subdomain 2 of the molecule is of critical importance for DNAase 1 binding and protein polymerization, while a very crucial C 374 residue and potential binding site for 4-HNE is present in the conformationally critical hydrophobic pocket of the molecule. Our findings indicate that the observed reduction in beta-actin band intensity is independent of the employed monoclonal antibodies and are compatible with a real decrease in the betaactin expression in the R patients erythrocytes membrane. Moreover, the reported evidence exhaustively addresses the question of whether the observed decrease in beta-actin protein expression might be related to oxidative PTMs potentially preventing antibody recognition. Taken together, our data indicate that major alterations exist in the beta-actin of R erythrocytes which results both from changes in expression and as a consequence of oxidative damage. To this regard, beta-actin is a well-known major target for OS processes, while erythrocytes represent ����cellular detectors���� revealing the co-existence of major cytoskeletal changes in this key genetic model for neurodevelopmental disorders. In particular, this work suggests a novel role for MeCP2 as a stabilizing protein in microtubule dynamics. To date, no definitive cure for R exists, although several approaches to a potential therapy have been either a empted or hypothesized, including activation of the silenced Mecp2 gene, gene therapy, modulation of some of the downstream effects from MeCP2-deficiency. Our study indicates that a proteomic approach in R is able to reveal additional downstream effects of the MECP2-deficiency, and therefore could identify potentially novel therapeutical targets for the disease. The four serotypes of dengue virus cause the most important arthropod-borne viral disease of humans. DENV infection results in a range of clinical outcomes ranging from the milder dengue fever to the potentially life threatening dengue haemorrhagic fever/dengue shock syndrome. A recent study estimates that up to 390 million people are infected with DENV annually, making dengue a serious global public-health problem. Despite much effort, there are neither vaccines nor antiviral therapies in clinical use to prevent or treat dengue, and our understanding of dengue pathogenesis is still limited. DENV is a member of the Flavivirus genus of the Flaviviridae family and has a RNA genome of,11 kb in size.
Many novel proteins not previously identified to be effected by DENV infection
Bioinformatic analysis was used to Praeruptorin-B identify a number of processes affected by DENV-2 infection. The results of the SILAC-MS analysis was validated for seven selected proteins by Western blo ing and immunofluorescence microscopy. This is the first report of the application of SILACMS  to study changes in the host cell proteome in response to DENV infection and demonstrates the power of this technique for identifying and quantifying changes in cellular protein amounts in response to DENV infection. In order to conduct the proteomic analysis, human lung carcinoma A549 cells were grown for eight cell doublings in either light or heavy Senegenin labeled media before being mock infected or infected with DENV-2 respectively. Although not believed to represent a target cell for DENV in vivo, A549 cells are highly permissive for DENV infection and have been used in previous studies examining the effect of DENV on the cellular innate immune response and the host cell transcriptome. At 28 hours p.i., a time point determined by growth curve analysis to lie in exponential phase of DENV replication, the cells were harvested and fractionated into nuclear and cytoplasmic extracts. At this time there was no obvious difference in the morphology of the mock and DENV infected cells, suggesting that there was li le cell death. IFA analysis of a sample of the mock and infected A549 cells revealed that 100% of the cells had been infected. The fractionation was done to reduce the overall complexity of the sample and to identify proteins that were altered in amount or redistributed between the cytoplasm and nucleus during DENV infection. DENV is known to replicate in tight association with perinuclear membranes therefore the cells were fractionated using a procedure that removed as much of the perinuclear membrane as possible without disrupting the nuclei. The presence of protein markers in the cellular fractions specific to the nucleus, cytoplasm and DENV infection were analyzed by Western blo ing to validate the infection and fractionation procedures. The analysis showed that whilst the nuclear and soluble cytoplasmic protein fractions were distinct, the lack of detergent in the lysis buffer led to the presence of some membraneous/ cytoskeletal proteins in the nuclear fractions. It appeared that the perinuclear membrane and the associated viral replication structures were not totally removed from the nuclei, as evidenced by a minor amount of the virus E protein, which is cytoplasmically localized, in the nuclear fraction. By contrast, the NS5 protein is known to be found in both the nucleus and cytoplasm of infected cells. Equal protein amounts from the cytoplasmic fractions of the mock and DENV-2 infected cells were pooled and the same procedure repeated for the nuclear fractions. The proteins in the cytoplasmic and nuclear fractions were separated by 1D SDSPAGE, subject to in-gel tryptic digestion and the peptides analyzed by quantitative LC-MS/MS to determine the relative amounts of proteins in the nuclear and cytoplasmic fractions from mock and DENV-2 infected cells. This procedure was done once and resulted in the identification of 4053 and 2881 cellular proteins in the cytoplasmic and nuclear fractions of which 3098 and 2115 respectively, were reliably quantified.
to study changes in the host cell proteome in response to DENV infection and demonstrates the power of this technique for identifying and quantifying changes in cellular protein amounts in response to DENV infection. In order to conduct the proteomic analysis, human lung carcinoma A549 cells were grown for eight cell doublings in either light or heavy Senegenin labeled media before being mock infected or infected with DENV-2 respectively. Although not believed to represent a target cell for DENV in vivo, A549 cells are highly permissive for DENV infection and have been used in previous studies examining the effect of DENV on the cellular innate immune response and the host cell transcriptome. At 28 hours p.i., a time point determined by growth curve analysis to lie in exponential phase of DENV replication, the cells were harvested and fractionated into nuclear and cytoplasmic extracts. At this time there was no obvious difference in the morphology of the mock and DENV infected cells, suggesting that there was li le cell death. IFA analysis of a sample of the mock and infected A549 cells revealed that 100% of the cells had been infected. The fractionation was done to reduce the overall complexity of the sample and to identify proteins that were altered in amount or redistributed between the cytoplasm and nucleus during DENV infection. DENV is known to replicate in tight association with perinuclear membranes therefore the cells were fractionated using a procedure that removed as much of the perinuclear membrane as possible without disrupting the nuclei. The presence of protein markers in the cellular fractions specific to the nucleus, cytoplasm and DENV infection were analyzed by Western blo ing to validate the infection and fractionation procedures. The analysis showed that whilst the nuclear and soluble cytoplasmic protein fractions were distinct, the lack of detergent in the lysis buffer led to the presence of some membraneous/ cytoskeletal proteins in the nuclear fractions. It appeared that the perinuclear membrane and the associated viral replication structures were not totally removed from the nuclei, as evidenced by a minor amount of the virus E protein, which is cytoplasmically localized, in the nuclear fraction. By contrast, the NS5 protein is known to be found in both the nucleus and cytoplasm of infected cells. Equal protein amounts from the cytoplasmic fractions of the mock and DENV-2 infected cells were pooled and the same procedure repeated for the nuclear fractions. The proteins in the cytoplasmic and nuclear fractions were separated by 1D SDSPAGE, subject to in-gel tryptic digestion and the peptides analyzed by quantitative LC-MS/MS to determine the relative amounts of proteins in the nuclear and cytoplasmic fractions from mock and DENV-2 infected cells. This procedure was done once and resulted in the identification of 4053 and 2881 cellular proteins in the cytoplasmic and nuclear fractions of which 3098 and 2115 respectively, were reliably quantified.
We therefore cannot exclude with certainty that there might have been selection of drug resistance
To this end, we compared the viral decay and the time to viral suppression between the early treated patients who reinitiated cART and the patients in whom treatment was deferred until conventional criteria to start long-term cART had been reached. Temporary cART during PHI did not select for clinically relevant drug resistance mutations and was associated with a durable and persisting virologic response after subsequent reinitiation of long-term cART. Our data thereby support the use of early treatment during PHI. Of note, the slower decline of the pVL from 8 weeks onward in the second treatment period of the early treated patients is probably an artefact of the model, because patients had a lower baseline pVL at restart than during early treatment and their pVL was usually already undetectable by week 8. 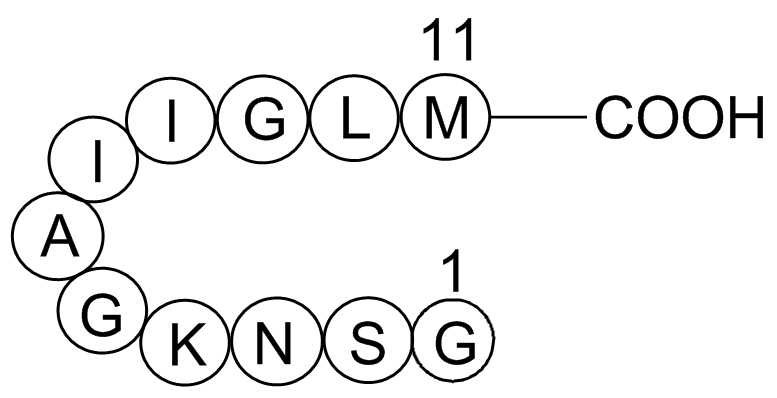 We were not able to perform resistance testing after TI in 7/63 of the early treated patients. This is in particular relevant for patients who interrupted an NNRTI-based regimen, because of the long half-life of NNRTIs. However, in all seven patients, irrespective of the regimen, the pVL was resuppressed upon restart, which virtually excludes clinically important mutations. The early treated patients reinitiated long-term cART more often with a boosted PI than naive patients. Many early treated patients preferred not to restart an NNRTI because of side-effects they had experienced previously during the early cART period, and therefore favoured a PI-containing regimen. Our study is supported by another study in which 37 PHIpatients were treated with temporary early cART and no drug resistance was observed after TI. However, in this study the NNRTI was stopped 96 h before the NRTI-backbone. Because NNRTIs have a slower metabolism and a low genetic barrier to resistance, simultaneous TI of an NNRTI-containing Albaspidin-AA regimen may result in a period of NNRTI-monotherapy, which may select for drug resistance mutations. NNRTI-drug resistance mutations that were selected after intrapartum exposure to single-dose nevirapine in HIV-infected women have been associated with decreased virologic response after subsequent treatment with an NNRTI-containing regimen. Noteworthy, the pVL in these women exposed to single-dose nevirapine was much higher than the pVL in a controlled TI-se ing in which patients have an undetectable pVL at TI. In the SMART trial, NNRTI-drug resistance mutations were more common in case of simultaneous TI than in case of a staggered or a switched interruption, in which the NNRTI is replaced by a boosted PI. However, in SMART most drug combinations included a zidovudine/lamivudine-backbone in combination with an NNRTI, whereas in our trial half of the patients were using a tenofovircontaining regimen, which has a longer half-life, and 20(S)-Notoginsenoside-R2 together with an NNRTI forms a more balanced regimen that is less prone to development of drug resistance when treatment is discontinued simultaneously. To date, there is no clear consensus how to stop cART regimens. In our study we found no indication for selection of drug resistance mutations after interrupting all drugs simultaneously once an undetectable pVL had been reached.
We were not able to perform resistance testing after TI in 7/63 of the early treated patients. This is in particular relevant for patients who interrupted an NNRTI-based regimen, because of the long half-life of NNRTIs. However, in all seven patients, irrespective of the regimen, the pVL was resuppressed upon restart, which virtually excludes clinically important mutations. The early treated patients reinitiated long-term cART more often with a boosted PI than naive patients. Many early treated patients preferred not to restart an NNRTI because of side-effects they had experienced previously during the early cART period, and therefore favoured a PI-containing regimen. Our study is supported by another study in which 37 PHIpatients were treated with temporary early cART and no drug resistance was observed after TI. However, in this study the NNRTI was stopped 96 h before the NRTI-backbone. Because NNRTIs have a slower metabolism and a low genetic barrier to resistance, simultaneous TI of an NNRTI-containing Albaspidin-AA regimen may result in a period of NNRTI-monotherapy, which may select for drug resistance mutations. NNRTI-drug resistance mutations that were selected after intrapartum exposure to single-dose nevirapine in HIV-infected women have been associated with decreased virologic response after subsequent treatment with an NNRTI-containing regimen. Noteworthy, the pVL in these women exposed to single-dose nevirapine was much higher than the pVL in a controlled TI-se ing in which patients have an undetectable pVL at TI. In the SMART trial, NNRTI-drug resistance mutations were more common in case of simultaneous TI than in case of a staggered or a switched interruption, in which the NNRTI is replaced by a boosted PI. However, in SMART most drug combinations included a zidovudine/lamivudine-backbone in combination with an NNRTI, whereas in our trial half of the patients were using a tenofovircontaining regimen, which has a longer half-life, and 20(S)-Notoginsenoside-R2 together with an NNRTI forms a more balanced regimen that is less prone to development of drug resistance when treatment is discontinued simultaneously. To date, there is no clear consensus how to stop cART regimens. In our study we found no indication for selection of drug resistance mutations after interrupting all drugs simultaneously once an undetectable pVL had been reached.
The phosphorylated form of tau is known to associate with tubulin to stabilize axonal microtubules
These included patient age, number of rib fractures, chronic lung disease and pre-injury anti-coagulant use. This is the first study in which pre-injury anti-platelet use has been reported as a risk factor for complications following isolated blunt chest wall trauma. Pathophysiological mechanisms differ substantially between blunt poly-trauma patients suffering trauma-induced coagulopathy and isolated blunt chest trauma patients and as a result, comparisons between such studies are not appropriate. The results of this study are therefore distinctive from any previous research and should be considered by emergency physicians managing isolated blunt chest trauma. Anti-platelet therapy is now a well-recognised risk factor for potential poor outcomes following Ganoderic-acid-F severe traumatic head Notoginsenoside-Fe injuries and trauma clinicians are becoming increasingly aware of its negative impact in the elderly trauma patient. Despite the limitations associated with a single centre retrospective study, this results of this study have highlighted an important clinical finding that trauma clinicians should  consider when managing the blunt chest wall trauma patient in the ED. A prospective multi-centre study is planned to further investigate the impact of pre-injury anti-platelet use on outcomes in blunt chest wall trauma patients. Microtubules are one of the major cytoskeletal components and play critical roles in diverse cellular events. While the dynamic property of microtubules is important for many microtubulemediated cellular events such as cell division and migration, the stability of microtubules is also important, especially for intracellular transport and the maintenance of cell polarity. Deregulation of microtubule stability can lead to severe consequences such as developmental defects and neurodegenerative diseases. In cells, microtubule stability is controlled by a number of proteins interacting with microtubules and/or its tubulin subunits, collectively known as microtubule-associated proteins. The level of Mdp3 varies significantly in different tissues, with relatively high expression in skeletal muscle and lung tissues. In addition, Mdp3 expression undergoes dramatic changes during the cell cycle, with lower expression in the G2 phase compared with its expression in the other phases of the cell cycle. It has been demonstrated previously that Mdp3 plays an important role in the regulation of microtubule stability. However, the molecular mechanisms underlying this function of Mdp3 remain unclear. In this study, we provide the first evidence that Mdp3 modulates microtubule stability via two different mechanisms, direct binding to microtubules/tubulin and regulating histone deacetylase 6 -mediated tubulin deacetylation. Proteins of the MAP family are key players in the regulation of microtubule stability. Abnormal expression or posttranslational modification of MAPs has been implicated in the pathogenesis of human diseases especially neurodegenerative diseases.
consider when managing the blunt chest wall trauma patient in the ED. A prospective multi-centre study is planned to further investigate the impact of pre-injury anti-platelet use on outcomes in blunt chest wall trauma patients. Microtubules are one of the major cytoskeletal components and play critical roles in diverse cellular events. While the dynamic property of microtubules is important for many microtubulemediated cellular events such as cell division and migration, the stability of microtubules is also important, especially for intracellular transport and the maintenance of cell polarity. Deregulation of microtubule stability can lead to severe consequences such as developmental defects and neurodegenerative diseases. In cells, microtubule stability is controlled by a number of proteins interacting with microtubules and/or its tubulin subunits, collectively known as microtubule-associated proteins. The level of Mdp3 varies significantly in different tissues, with relatively high expression in skeletal muscle and lung tissues. In addition, Mdp3 expression undergoes dramatic changes during the cell cycle, with lower expression in the G2 phase compared with its expression in the other phases of the cell cycle. It has been demonstrated previously that Mdp3 plays an important role in the regulation of microtubule stability. However, the molecular mechanisms underlying this function of Mdp3 remain unclear. In this study, we provide the first evidence that Mdp3 modulates microtubule stability via two different mechanisms, direct binding to microtubules/tubulin and regulating histone deacetylase 6 -mediated tubulin deacetylation. Proteins of the MAP family are key players in the regulation of microtubule stability. Abnormal expression or posttranslational modification of MAPs has been implicated in the pathogenesis of human diseases especially neurodegenerative diseases.