To this end, we compared the viral decay and the time to viral suppression between the early treated patients who reinitiated cART and the patients in whom treatment was deferred until conventional criteria to start long-term cART had been reached. Temporary cART during PHI did not select for clinically relevant drug resistance mutations and was associated with a durable and persisting virologic response after subsequent reinitiation of long-term cART. Our data thereby support the use of early treatment during PHI. Of note, the slower decline of the pVL from 8 weeks onward in the second treatment period of the early treated patients is probably an artefact of the model, because patients had a lower baseline pVL at restart than during early treatment and their pVL was usually already undetectable by week 8. 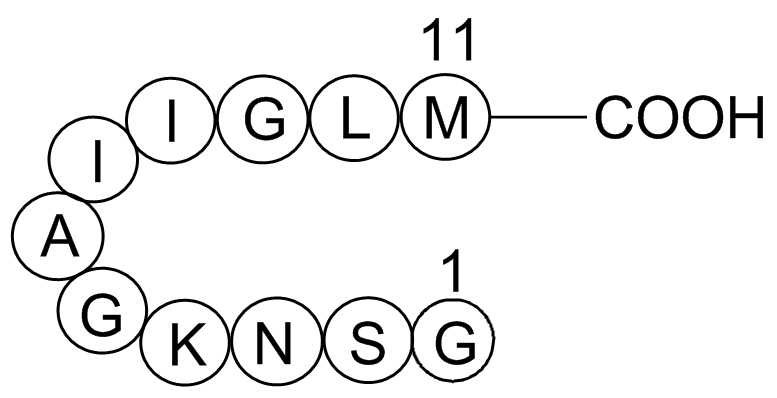 We were not able to perform resistance testing after TI in 7/63 of the early treated patients. This is in particular relevant for patients who interrupted an NNRTI-based regimen, because of the long half-life of NNRTIs. However, in all seven patients, irrespective of the regimen, the pVL was resuppressed upon restart, which virtually excludes clinically important mutations. The early treated patients reinitiated long-term cART more often with a boosted PI than naive patients. Many early treated patients preferred not to restart an NNRTI because of side-effects they had experienced previously during the early cART period, and therefore favoured a PI-containing regimen. Our study is supported by another study in which 37 PHIpatients were treated with temporary early cART and no drug resistance was observed after TI. However, in this study the NNRTI was stopped 96 h before the NRTI-backbone. Because NNRTIs have a slower metabolism and a low genetic barrier to resistance, simultaneous TI of an NNRTI-containing Albaspidin-AA regimen may result in a period of NNRTI-monotherapy, which may select for drug resistance mutations. NNRTI-drug resistance mutations that were selected after intrapartum exposure to single-dose nevirapine in HIV-infected women have been associated with decreased virologic response after subsequent treatment with an NNRTI-containing regimen. Noteworthy, the pVL in these women exposed to single-dose nevirapine was much higher than the pVL in a controlled TI-se ing in which patients have an undetectable pVL at TI. In the SMART trial, NNRTI-drug resistance mutations were more common in case of simultaneous TI than in case of a staggered or a switched interruption, in which the NNRTI is replaced by a boosted PI. However, in SMART most drug combinations included a zidovudine/lamivudine-backbone in combination with an NNRTI, whereas in our trial half of the patients were using a tenofovircontaining regimen, which has a longer half-life, and 20(S)-Notoginsenoside-R2 together with an NNRTI forms a more balanced regimen that is less prone to development of drug resistance when treatment is discontinued simultaneously. To date, there is no clear consensus how to stop cART regimens. In our study we found no indication for selection of drug resistance mutations after interrupting all drugs simultaneously once an undetectable pVL had been reached.
We were not able to perform resistance testing after TI in 7/63 of the early treated patients. This is in particular relevant for patients who interrupted an NNRTI-based regimen, because of the long half-life of NNRTIs. However, in all seven patients, irrespective of the regimen, the pVL was resuppressed upon restart, which virtually excludes clinically important mutations. The early treated patients reinitiated long-term cART more often with a boosted PI than naive patients. Many early treated patients preferred not to restart an NNRTI because of side-effects they had experienced previously during the early cART period, and therefore favoured a PI-containing regimen. Our study is supported by another study in which 37 PHIpatients were treated with temporary early cART and no drug resistance was observed after TI. However, in this study the NNRTI was stopped 96 h before the NRTI-backbone. Because NNRTIs have a slower metabolism and a low genetic barrier to resistance, simultaneous TI of an NNRTI-containing Albaspidin-AA regimen may result in a period of NNRTI-monotherapy, which may select for drug resistance mutations. NNRTI-drug resistance mutations that were selected after intrapartum exposure to single-dose nevirapine in HIV-infected women have been associated with decreased virologic response after subsequent treatment with an NNRTI-containing regimen. Noteworthy, the pVL in these women exposed to single-dose nevirapine was much higher than the pVL in a controlled TI-se ing in which patients have an undetectable pVL at TI. In the SMART trial, NNRTI-drug resistance mutations were more common in case of simultaneous TI than in case of a staggered or a switched interruption, in which the NNRTI is replaced by a boosted PI. However, in SMART most drug combinations included a zidovudine/lamivudine-backbone in combination with an NNRTI, whereas in our trial half of the patients were using a tenofovircontaining regimen, which has a longer half-life, and 20(S)-Notoginsenoside-R2 together with an NNRTI forms a more balanced regimen that is less prone to development of drug resistance when treatment is discontinued simultaneously. To date, there is no clear consensus how to stop cART regimens. In our study we found no indication for selection of drug resistance mutations after interrupting all drugs simultaneously once an undetectable pVL had been reached.
Month: April 2019
The phosphorylated form of tau is known to associate with tubulin to stabilize axonal microtubules
These included patient age, number of rib fractures, chronic lung disease and pre-injury anti-coagulant use. This is the first study in which pre-injury anti-platelet use has been reported as a risk factor for complications following isolated blunt chest wall trauma. Pathophysiological mechanisms differ substantially between blunt poly-trauma patients suffering trauma-induced coagulopathy and isolated blunt chest trauma patients and as a result, comparisons between such studies are not appropriate. The results of this study are therefore distinctive from any previous research and should be considered by emergency physicians managing isolated blunt chest trauma. Anti-platelet therapy is now a well-recognised risk factor for potential poor outcomes following Ganoderic-acid-F severe traumatic head Notoginsenoside-Fe injuries and trauma clinicians are becoming increasingly aware of its negative impact in the elderly trauma patient. Despite the limitations associated with a single centre retrospective study, this results of this study have highlighted an important clinical finding that trauma clinicians should  consider when managing the blunt chest wall trauma patient in the ED. A prospective multi-centre study is planned to further investigate the impact of pre-injury anti-platelet use on outcomes in blunt chest wall trauma patients. Microtubules are one of the major cytoskeletal components and play critical roles in diverse cellular events. While the dynamic property of microtubules is important for many microtubulemediated cellular events such as cell division and migration, the stability of microtubules is also important, especially for intracellular transport and the maintenance of cell polarity. Deregulation of microtubule stability can lead to severe consequences such as developmental defects and neurodegenerative diseases. In cells, microtubule stability is controlled by a number of proteins interacting with microtubules and/or its tubulin subunits, collectively known as microtubule-associated proteins. The level of Mdp3 varies significantly in different tissues, with relatively high expression in skeletal muscle and lung tissues. In addition, Mdp3 expression undergoes dramatic changes during the cell cycle, with lower expression in the G2 phase compared with its expression in the other phases of the cell cycle. It has been demonstrated previously that Mdp3 plays an important role in the regulation of microtubule stability. However, the molecular mechanisms underlying this function of Mdp3 remain unclear. In this study, we provide the first evidence that Mdp3 modulates microtubule stability via two different mechanisms, direct binding to microtubules/tubulin and regulating histone deacetylase 6 -mediated tubulin deacetylation. Proteins of the MAP family are key players in the regulation of microtubule stability. Abnormal expression or posttranslational modification of MAPs has been implicated in the pathogenesis of human diseases especially neurodegenerative diseases.
consider when managing the blunt chest wall trauma patient in the ED. A prospective multi-centre study is planned to further investigate the impact of pre-injury anti-platelet use on outcomes in blunt chest wall trauma patients. Microtubules are one of the major cytoskeletal components and play critical roles in diverse cellular events. While the dynamic property of microtubules is important for many microtubulemediated cellular events such as cell division and migration, the stability of microtubules is also important, especially for intracellular transport and the maintenance of cell polarity. Deregulation of microtubule stability can lead to severe consequences such as developmental defects and neurodegenerative diseases. In cells, microtubule stability is controlled by a number of proteins interacting with microtubules and/or its tubulin subunits, collectively known as microtubule-associated proteins. The level of Mdp3 varies significantly in different tissues, with relatively high expression in skeletal muscle and lung tissues. In addition, Mdp3 expression undergoes dramatic changes during the cell cycle, with lower expression in the G2 phase compared with its expression in the other phases of the cell cycle. It has been demonstrated previously that Mdp3 plays an important role in the regulation of microtubule stability. However, the molecular mechanisms underlying this function of Mdp3 remain unclear. In this study, we provide the first evidence that Mdp3 modulates microtubule stability via two different mechanisms, direct binding to microtubules/tubulin and regulating histone deacetylase 6 -mediated tubulin deacetylation. Proteins of the MAP family are key players in the regulation of microtubule stability. Abnormal expression or posttranslational modification of MAPs has been implicated in the pathogenesis of human diseases especially neurodegenerative diseases.
It has been widely accepted that miRNAs play pivotal in various biological processes associated with reduced vitamin B12 levels
Defects in the C1-tetrahydrofolate metabolic pathway may decrease the levels of vitamin B12. It is possible that the inconsistent findings associating rs6922269 with various heart disease phenotypes in this and other studies may be due in part to MTHFD1L gene-environment interactions, particularly dietary variation in folate content leading to variation in folate metabolite levels and therefore risks of disease progression. Folate status and drug treatment regimen have undergone substantial changes in New Zealand during the decade between the median dates of recruitment for each cohort. However it must be acknowledge that this interpretation of the data is circumstantial and as such should be viewed as hypothesis generating. Further studies of the utility of rs6922269 as a diagnostic and prognostic marker in CHD patients are needed, with particular emphasis on participants’ dietary intake and nutritional status, especially folate pathway metabolites. While a recent large meta-analysis of GWAS markers for dyslipidaemia, Coptisine-chloride diabetes and CHD found rs6922269 was associated with CHD risk, investigation of the association of rs6922269 with survival  in patients with established CAD has been limited. A recent GWAS of mortality after ACS identified rs6922269 as the only SNP of 95 investigated to achieve Bonferroni-corrected significant association with mortality in the test cohort. This finding was replicated in the African-American subgroup of a second cohort, but not in two additional independent cohorts, resonant with our own results. Gastric cancer is one of the most common malignant diseases worldwide. The prognosis of gastric cancer is poor and patients are generally diagnosed at a rather advanced stage in most countries. Thus, the overall 5-year survival rate is about 40%, and that of the patients with distant metastasis is less than 5%. Approximately 700,000 gastric cancer patients die annually, making it the second most common cause of cancerrelated death worldwide. Data showed that the crude mortality rate of gastric cancer was 25.2 per 100,000. But there exists remarkable geographical variation in incidence of gastric cancer for eastern countries such as China and Japan have highest rates of gastric cancer than western countries. In China, gastric cancer is the second most frequently diagnosed cancer and the third leading cause of cancer death, with an estimated 464 439 new cases and 352 315 cancer deaths in 2008. The overall estimated age-adjusted incidence rate in 2008 was 29.9 per 100,000 people in China. So, gastric cancer remains a significant problem worldwide despite a declining incidence in not only western countries but also China. MicroRNAs are a class of highly conserved, singlestranded, small noncoding RNA molecules, which are known as endogenous regulators of post-transcriptional gene expression regulating expression through translational repression and messenger RNA cleavage. They can inhibit gene expression at the posttranscriptional level by binding to the 39 Saikosaponin-C untranslated region of target mRNAs can result in mRNA degradation or translation inhibition, depending on the degree of complementary base pairing.
in patients with established CAD has been limited. A recent GWAS of mortality after ACS identified rs6922269 as the only SNP of 95 investigated to achieve Bonferroni-corrected significant association with mortality in the test cohort. This finding was replicated in the African-American subgroup of a second cohort, but not in two additional independent cohorts, resonant with our own results. Gastric cancer is one of the most common malignant diseases worldwide. The prognosis of gastric cancer is poor and patients are generally diagnosed at a rather advanced stage in most countries. Thus, the overall 5-year survival rate is about 40%, and that of the patients with distant metastasis is less than 5%. Approximately 700,000 gastric cancer patients die annually, making it the second most common cause of cancerrelated death worldwide. Data showed that the crude mortality rate of gastric cancer was 25.2 per 100,000. But there exists remarkable geographical variation in incidence of gastric cancer for eastern countries such as China and Japan have highest rates of gastric cancer than western countries. In China, gastric cancer is the second most frequently diagnosed cancer and the third leading cause of cancer death, with an estimated 464 439 new cases and 352 315 cancer deaths in 2008. The overall estimated age-adjusted incidence rate in 2008 was 29.9 per 100,000 people in China. So, gastric cancer remains a significant problem worldwide despite a declining incidence in not only western countries but also China. MicroRNAs are a class of highly conserved, singlestranded, small noncoding RNA molecules, which are known as endogenous regulators of post-transcriptional gene expression regulating expression through translational repression and messenger RNA cleavage. They can inhibit gene expression at the posttranscriptional level by binding to the 39 Saikosaponin-C untranslated region of target mRNAs can result in mRNA degradation or translation inhibition, depending on the degree of complementary base pairing.
It is in this increasing elderly population where antiplatelet drug use is more prevalent
As a result of this increased use of anti-platelet therapy as the population ages, it is vital that trauma clinicians understand the risks involved with their use. Pre-injury anti-platelet use has been increasingly investigated as a risk factor for various poor outcomes in traumatic head injuries. A number of studies have concluded that anti-platelet therapy is a risk factor for both shortterm and Forsythin long-term unfavourable outcomes in subjects with head injury, with increased risk of death, permanent vegetative state and severe disability. A further difficulty currently facing trauma clinicians is that limited research exists that addresses the efficacy or utility of reversing pre-injury anti-platelets therapy in traumatic head injury.. Another difficulty facing emergency physicians in the management of trauma patients using pre-injury anti-platelets is the variation between patients in their response to the medication. Platelet function tests can be carried out on trauma patients in order to assess number and size of platelets and also platelet haemostatic function. The type of tests completed, specifically either global screening tests or specific assays will depend on the testing equipment available at that emergency department. The decision as to whether the blunt poly-trauma patient requires platelet transfusion therefore is dependent on a number of factors. In isolated blunt chest trauma however platelet function may not routinely be considered by the emergency physician even though delayed haemothorax is not an uncommon entity in this patient group. It could  be suggested that tests for platelet function may be an important consideration for the emergency physician managing the isolated blunt chest trauma patient however further research is required to support this suggestion. To date, no research exists investigating the effect of pre-injury anti-platelet use in blunt chest trauma. Pulmonary contusion occurs in 25�C35% of all blunt chest traumas and is defined as an injury to the alveolar capillaries, in the absence of a lung laceration. This results in accumulation of blood and other fluids within the lung tissue which subsequently interferes with gas exchange leading to hypoxia. If blood and plasma are leaked into the alveoli in rib fractures patients, it Alisol-A-24-acetate possible that this pathophysiological process is exacerbated in patients receiving preinjury anti-platelet therapy. This variable has not been investigated to date as a risk factor for poor outcomes following blunt chest wall trauma. In one previous study, pre-injury anti-platelet therapy was reported to reduce the incidence of acute lung injury in a medical ICU population, of which there were 24 poly-trauma patients in the study cohort and only eight of these were using preinjury anti-platelets. The authors of this study also do not state whether these trauma patients had sustained head injuries and therefore comparison between the studies is not possible. In a recent study by Harr et al, the use of pre-injury antiplatelet therapy was reported to be associated with a decreased risk of lung dysfunction in high risk blunt trauma patients who receive blood transfusions.
be suggested that tests for platelet function may be an important consideration for the emergency physician managing the isolated blunt chest trauma patient however further research is required to support this suggestion. To date, no research exists investigating the effect of pre-injury anti-platelet use in blunt chest trauma. Pulmonary contusion occurs in 25�C35% of all blunt chest traumas and is defined as an injury to the alveolar capillaries, in the absence of a lung laceration. This results in accumulation of blood and other fluids within the lung tissue which subsequently interferes with gas exchange leading to hypoxia. If blood and plasma are leaked into the alveoli in rib fractures patients, it Alisol-A-24-acetate possible that this pathophysiological process is exacerbated in patients receiving preinjury anti-platelet therapy. This variable has not been investigated to date as a risk factor for poor outcomes following blunt chest wall trauma. In one previous study, pre-injury anti-platelet therapy was reported to reduce the incidence of acute lung injury in a medical ICU population, of which there were 24 poly-trauma patients in the study cohort and only eight of these were using preinjury anti-platelets. The authors of this study also do not state whether these trauma patients had sustained head injuries and therefore comparison between the studies is not possible. In a recent study by Harr et al, the use of pre-injury antiplatelet therapy was reported to be associated with a decreased risk of lung dysfunction in high risk blunt trauma patients who receive blood transfusions.
The formation of disulfide-bond containing proteins in bacterial cytosol is unstable
For the expression of proteins containing disulfide bonds and normally forms inactive inclusion bodies. Therefore, additional in-vitro refolding is required to obtain biologically functional proteins. However, it is well known that invitro refolding of Eleutheroside-E protein in inclusion bodies is often unpredictable and challenging, in addition to being time consuming and requiring a large amount of reagents. Overall, generation of protein in soluble form is the preferred choice. Extensive efforts have been made to overcome these obstacles to improve soluble expression of different disulfide-bonded proteins in the cytosol of E. coli. Cysteines in the E. coli cytoplasm are actively kept reduced by pathways involving thioredoxin reductase and glutaredoxin, so one strategy is to alter these reducing pathways to change the cytoplasmic thiol-redox equilibrium environment. In the current work, a TRX fusion tag was attached to the Nterminus of the FGF19 and FGF15 protein, then the fusion proteins were expressed in various E. coli mutant Ganoderic-acid-F strains, and soluble protein expression in bacteria cytoplasm were determined. Previous studies have shown no post-translational modification in mature FGF15 and FGF19 proteins, indicating that the bacterial system could be used for expression of both proteins. However, both proteins contain two disulfide bonds, suggesting that they may be expressed as insoluble inclusion bodies due to the lack of ability to form disulfide bond in the reducing environment of E. coli cytoplasm. With the modification of the cytoplasmic reducing environment and co-expression of fusion protein TRX chaperones, soluble FGF19 protein can be expressed in bacterial cytosol, and this result is consistent with a previous finding showing that thioredoxin can improve disulfide bond formation in a reducing background. Interestingly, co-expression of DsbC alone in the reducing environment of the cytoplasm was sufficient to improve FGF19 solubility.  Disulfide isomerase is a periplasmic enzyme that catalyzes the isomerization of disulfide bonds. DsbC has been found to function as a chaperone to improve the solubility of disulfide bonds containing proteins in E. coli cytoplasm. This could also explain why TRX fusion protein in the presence of DsbC would further improve FGF19 solubility. However, modification of the reducing environment and co-expression with these chaperones did not help produce satisfactory quantities of soluble FGF15 protein, indicating that other factors may be critical for its soluble expression. Moreover, it’s well known that every species has codon usage bias, and differences in codon usage can impede translation due to shortage or lacking for one or more tRNAs when heterologous proteins are overexpressed in E. coli. Plasmids of pRARE2 from Rosettagami 2 cells, which supplies tRNAs for seven rare codons, were isolated and cotransfected with the FGF15 and FGF19 expression plasmids into SHuffle T7 E. coli strains, but the results showed that overexpression of the rare tRNAs had no effect on the FGF15 and FGF19 solubility in the cytoplasm, indicating that codon bias is not the major reason to prevent FG15 soluble expression. More studies need to be performed to determine the mechanism. Because both FGF15 and FGF19 have been shown to suppress the expression of the Cyp7a1 gene that is critical in bile acid synthesis through activating its receptor, FGFR4, they were predicted to have the same features. However, the FGF15 protein only shares 50% sequence homology with FGF19; moreover, our results showed that it’s much easier to express soluble FGF19 protein or refold FGF19 protein from inclusion bodies than those for FGF15 protein, indicating that there might be a greater difference between these two proteins than expected.
Disulfide isomerase is a periplasmic enzyme that catalyzes the isomerization of disulfide bonds. DsbC has been found to function as a chaperone to improve the solubility of disulfide bonds containing proteins in E. coli cytoplasm. This could also explain why TRX fusion protein in the presence of DsbC would further improve FGF19 solubility. However, modification of the reducing environment and co-expression with these chaperones did not help produce satisfactory quantities of soluble FGF15 protein, indicating that other factors may be critical for its soluble expression. Moreover, it’s well known that every species has codon usage bias, and differences in codon usage can impede translation due to shortage or lacking for one or more tRNAs when heterologous proteins are overexpressed in E. coli. Plasmids of pRARE2 from Rosettagami 2 cells, which supplies tRNAs for seven rare codons, were isolated and cotransfected with the FGF15 and FGF19 expression plasmids into SHuffle T7 E. coli strains, but the results showed that overexpression of the rare tRNAs had no effect on the FGF15 and FGF19 solubility in the cytoplasm, indicating that codon bias is not the major reason to prevent FG15 soluble expression. More studies need to be performed to determine the mechanism. Because both FGF15 and FGF19 have been shown to suppress the expression of the Cyp7a1 gene that is critical in bile acid synthesis through activating its receptor, FGFR4, they were predicted to have the same features. However, the FGF15 protein only shares 50% sequence homology with FGF19; moreover, our results showed that it’s much easier to express soluble FGF19 protein or refold FGF19 protein from inclusion bodies than those for FGF15 protein, indicating that there might be a greater difference between these two proteins than expected.